Releasing the brakes on the immune system: how a precision trick might help fight tumours
Regulatory T cells (Treg cells) are key immune cells that prevent excessive inflammation and autoimmunity by suppressing immune responses when they are no longer needed. To carry out this moderating role, Treg cells rely on the transcription factor Foxp3, long considered essential for Treg cell identity and function. However, whether mature Treg cells always require Foxp3—or only when responding to immune threats—has remained a mystery. Researchers from Joris van der Veeken’s lab at the IMP have now shown that Foxp3 is indispensable during inflammation. They also found that selectively breaking down Foxp3 triggers a strong anti-tumour immune response without harmful side effects, making it a promising target for cancer immunotherapy. Their findings are published in the journal Science Immunology.
When our immune system is triggered—by infection, injury, or even cancer—it launches a coordinated defence to eliminate the threat. But an immune response that goes unchecked can do more harm than good.
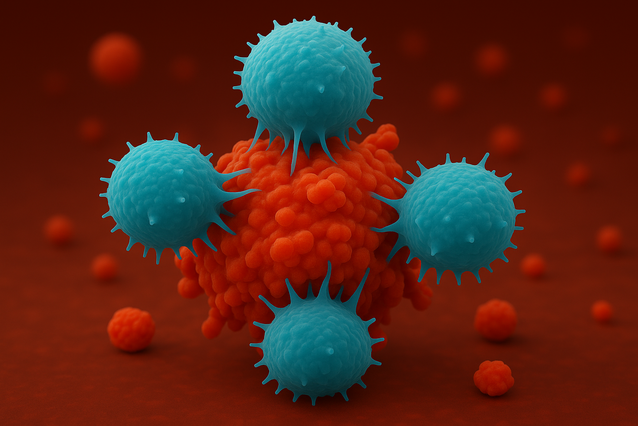
Regulatory T cells (Treg cells) act as critical moderators in this process, functioning much like the immune system’s brakes. Once the threat has passed, Treg cells suppress other immune cells to prevent excessive inflammation and autoimmune reactions. Without this crucial regulation, the immune system can spiral into uncontrolled activity, attacking the body’s own tissues.
Treg cells are defined by the expression of Foxp3, a transcription factor often referred to as their “master regulator”. Foxp3 has been studied for over a decade and is known to play a key role in maintaining a healthy immune system. When the gene responsible for Foxp3 production is mutated, this balance breaks down—leading to severe, often fatal autoimmune disease.
While Foxp3 gives regulatory T cells their identity, scientists still don’t know whether these cells rely on it continuously—or only when responding to inflammation. Answering this question has been challenging because traditional methods for studying gene function have key limitations.
Most traditional genetic tools, like gene knockouts, permanently delete a gene from the cell. But removing Foxp3 this way interferes with the early development of Treg cells, causing confounding defects that make it difficult to study the gene’s specific role in mature cells.
To tackle this problem, researchers in the lab of Joris van der Veeken at the IMP used a new method that triggers the precise breakdown of the key transcription factor with controlled short timing. They showed that Foxp3 is essential only during inflammation, when Treg cells are activated. The scientists also found that breaking down Foxp3 triggers a strong anti-tumour immune response without harmful side effects, suggesting a potential safe and effective target for improving cancer immunotherapy. Their findings are published in the journal Science Immunology.
Boosting cancer immunity one protein at a time
To study the role of Foxp3 with precision, Van der Veeken’s team used the auxin-inducible degron 2 (Aid2) system, a powerful tool that allows proteins to be selectively broken down. Originally developed for use in cell culture, they applied the method to study protein function in live mice. The system works by tagging the target protein so it can be recognised and destroyed, but only when a specific molecule—auxin, a plant hormone not naturally found in animals—is added. This makes it possible to control exactly when and where a protein is removed, without affecting the rest of the organism.
By temporarily removing Foxp3, the team was able to pinpoint when Treg cells truly rely on it. “Foxp3 is what defines Treg cells, but we were surprised to find it’s not always essential—at least in healthy conditions. Treg cells continue to function even without it.” says Christina Jäger, first author of the study and a student in the Vienna BioCenter PhD Program. “But in inflammatory environments—such as during infection, autoimmunity, or cancer—Foxp3 becomes critical for Treg cell survival and function.”
Because of this, removing Foxp3 in the whole body only affected the Treg cells inside tumours, where they were active, and not in healthy tissues. The researchers found that this triggered a powerful immune response specifically in tumours. “To our surprise, the treatment boosted anti-tumour immunity without causing harmful side effects,” says Jäger. “Without these cells acting as brakes, the immune system becomes more active in the tumour, slowing its growth—but without triggering harmful inflammation elsewhere in the body.”
The scientists suggest that targeting Foxp3 could be a safe and effective strategy for cancer immunotherapy, paving the way for more precise ways of controlling the immune system against disease—whether to boost it against cancer or calm it in autoimmunity.
“These discoveries were only possible thanks to the rapid and precise protein breakdown technique we used—something older methods couldn’t achieve,” says Joris van der Veeken, Group Leader at the IMP. “This method also gives scientists a powerful way to test immunotherapy candidates early on, before committing to full-scale drug development.”
Original Publication
Christina Jäger, Polina Dimitrova, Qiong Sun, Jesse Tennebroek, Elisa Marchiori, Markus Jaritz, Rene Rauschmeier, Guillem Estivill, Anna Obenauf, Meinrad Busslinger, and Joris van der Veeken#. “Inducible protein degradation reveals inflammation-dependent function of the Treg cell lineage-defining transcription factor Foxp3.” Science Immunology, DOI: 10.1126/sciimmunol.adr7057
#Corresponding author.
Further reading
Vienna BioCenter PhD Program
About the IMP at the Vienna BioCenter
The Research Institute of Molecular Pathology (IMP) in Vienna is a basic life science research institute largely sponsored by Boehringer Ingelheim. With over 220 scientists from 40 countries, the IMP is committed to scientific discovery of fundamental molecular and cellular mechanisms underlying complex biological phenomena. The IMP is part of the Vienna BioCenter, one of Europe’s most dynamic life science hubs with 2,800 people from over 80 countries in six research institutions, two universities, and 35 biotech companies. www.imp.ac.at, www.viennabiocenter.org